The experimental treatment deprived the patient of H.M. the possibility of creating memories. His case revolutionized research on memory. Who was he?
When Henry Molaison was a child, he survived an accident. Hospitals and care centers by the end of his days became a second home for him. Years of research have resulted in scientists getting to know Molaison's brain inside out . And with it - memory loss mechanisms . How did it come about? And why do medical documents mainly show male initials?
Childhood accident
Keeping an eye on a seven-year-old - almost impossible. Especially if we add a bicycle to it. In Henry's case, it didn't stop with scratches. Two versions of what actually happened in his childhood can be found. According to the first, the boy fell so unfortunately that he suffered a head injury . The second assumes that the accident was caused by a cyclist who ran into a child . Whatever happened then, determined Molaison's entire life. Some doctors saw the cause of epilepsy in the accident he struggled with over the years.
The disease developed gradually. Henry only experienced partial epilepsy as a child. They are characterized primarily by keeping consciousness. There may be hallucinations and delusions about the other senses , false sense of movement, déjà vu, speech disorders and misperceptions of space . The entire event takes no more than two minutes. It is usually memorized in detail.
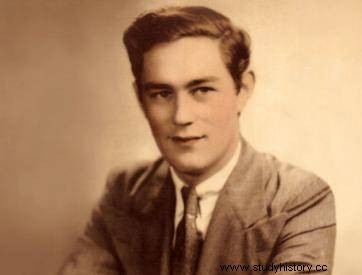
Henry Molaison before surgery
Unfortunately, as time went on, epilepsy became more and more severe. After his 16th birthday, Henry started having full epilepsy with loss of consciousness, convulsions and uncontrolled muscle contractions . Anticonvulsants allowed him to finish school and work on the assembly line. However, at the age of 27, the man overwhelmed the disease to such an extent that he was forced to seek other treatment options.
Effects of brain surgery
Molaison didn't have many options. At that time, epilepsy treatment methods did not bring almost any results . The frequency and strength of the seizures made it practically impossible for the young man to function normally. The only alternative was Dr. William Beecher Scoville's experimental method .
At that time, the scientist was working on a breakthrough therapy for epilepsy. Treatment was to remove the seizure areas of the brain . The operations carried out so far have actually resulted in this. But there was a problem with Scoville's research. All of his patients on whom he tested this method suffered from schizophrenia and psychosis. Their condition was improving. However, it was still a mystery what side effects could affect a fully conscious and sane person.
The only alternative was the experimental method of Dr. William Beecher Scoville (illustrative photo).
Molaison took the risk. Both he and his family consented to Operation . On September 1, 1953, a neurosurgeon removed 8 cm of brain tissue at Hartford Hospital . The excised portions comprised the hippocampus, and also fragments in the amygdala and entorhinal cortex. What do all these areas have in common? As we know today - each of them is somehow related to human memory.
The method developed by Dr. Scoville is used today. However, almost 70 years ago it was like wandering in the dark. The current technology enables incomparably more precise laser surgery to be performed . Moreover, the doctors of the time were not entirely sure which part of the brain was responsible for what. And the operation of memory was a mystery.
Lost memories
The treatment brought the basic assumed effect. The number of epilepsy attacks in a man has significantly decreased . Unfortunately, this is where the positives end. When Molaison recovered, remembers almost nothing about the two years before the operation . Some of the gaps even reached 11 years ago! However, everything that the man had experienced as a child remained intact. Nowadays, some researchers assume that the loss of memory could also be related to the frequency of seizures and various combinations of anticonvulsants.
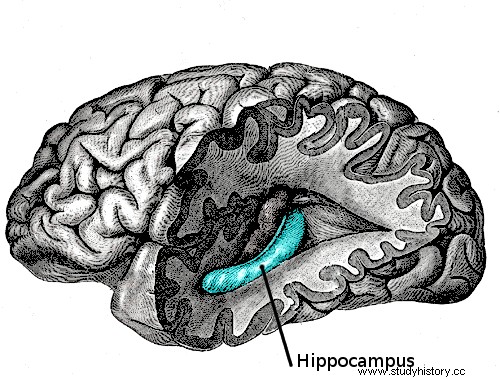
The excised parts comprised the hippocampus, and also fragments in the amygdala and entorhinal cortex.
Molaison was also unable to create new memories which was indisputably a consequence of the operation. He experienced each subsequent day for the first time. Sam once compared this feeling to "constantly waking up from sleep." How did it look like? Doctors and nurses had to introduce themselves to him every day. Several minutes after reading the newspaper, he could use it again. Besides, he had trouble recognizing himself in photos. He didn't notice how his face was visibly aging.
Mysterious patient H.M.
The man spent the rest of his life in a care center. Over the next decades it was subjected to various tests and studies . The tragedy that struck him and his family turned out to be a real breakthrough for science. He was the first non-psychotic patient with significant postoperative memory deficits. He was listed in medical records and articles as "patient H.M." . Why? It was primarily about the protection of personal data. The case of the man quickly became the subject of scientific publications. The use of first and last names would be problematic in this case. Molaison would simply not remember having consented to it. His details were only released after his death.
What exactly happened to him? To understand this, it is necessary to distinguish explicit memory from implicit (procedural). The first concerns factual knowledge, the second - the acquired skills. As it turned out, while H.M. he was unable to say what he had been doing the day before, so he learned to perform new activities without much problem. Procedural memory worked well for him. General mental abilities measured e.g. intelligence tests also did not change.
Life without explicit memory
Those who worked with patient H.M. described him as an upright, apparently confused man. In almost every situation, he looked for points of reference that would somehow help him find his way back in time. Perhaps crosswords helped him, which he willingly solved. And as far as they pertained to the knowledge prior to his surgery, he was pretty good at dealing with them. He was able to remember new facts very rudely without details. And only if they related somehow to things he knew before.
He had no problem with learning what to do. One of the tests that investigated this was to combine the points to form a star. The task was made much more difficult by the fact that the image could only be seen in a mirror image. With each attempt, Molaison did it better and better, although it always seemed to be his first time.

The personal tragedy of a man and his family turned out to be a breakthrough for science. (illustrative photo)
The personal tragedy of a man and his family turned out to be a breakthrough for science. Especially for Suzanne Corkin, who has been researching the functioning of Molaison over several decades until his death. The case of the patient H.M. confirmed that different areas of the brain are responsible for different types of memory. Working with a man has become the basis for further research on Alzheimer's, learning methods and retrieving lost memories.
Henry Molaison died in 2008. In addition to hundreds of pages of scientific reports, he left behind brain scans. And also… the very organ Corkin chose to remove and keep for research purposes.
